|
|
Thoracoplasty
Older Methods of Treating Tuberculosis
General considerations
- Defined as a “remodeling or reshaping of the thorax; especially, the operation of removing the ribs, so as to obliterate the pleural cavity in cases of empyema”
- Thoracoplasty was used from the early 1900’s through the late 1950’s as one of the more permanent forms of collapse therapy for TB
- Frequently used as a last resort in gravely ill patients
- Collapse therapy was based, at least in part, on the observation that healed tuberculous cavities were closed and not open
- The therapies were directed towards closing the cavities
- When this procedure was relatively common, the average TB patient required removal of 6-8 ribs
- This was frequently done in stages of 2-3 ribs per operation
- The remaining chest cage was then pushed toward the mediastinum, passively collapsing the upper lobe
- Thoracoplasty for TB was replaced by anti-tuberculous drugs
- Surgical treatments of TB were later directed at resection of the diseased portion of the lung instead of collapsing it
- Thoracoplasty is still used for chronic infections of the pleural space and as surgery in patients with scoliosis
Imaging findings
- The procedure results in a fairly characteristic deformity of the upper thoracic cage in which the first several ribs are displaced towards the mediastinum
- The chest cage then usually funnels out near the diaphragm to its normal shape
- The upper lobe is usually completely opacified and the remainder of the hemithorax may or may not demonstrate aerated lung, depending on the degree of fibrosis that developed
Other early treatments of TB
- Early treatments of TB relied upon rest, proper nutrition and isolation
- In late 1800’s, the concept of artificial pneumothorax was introduced by Carlo Forlanini of Milan
- Speculated on the feasibility of collapsing lung by introducing air into the pleural space
- Intentional production of a lung collapse was thought to allow the lung to rest
- It usually did nothing except possibly to worsen the condition of the patient
- By early ‘40s, thousands of refills (reinjections of air) were being done each year to maintain the collapsed lung
- Pneumoperitoneum to rest the lung followed in the late 1940s
- These techniques were often combined with phrenicolysis (crushing or surgical division of the phrenic nerve) leading to ipsilateral paralysis of the diaphragm
- Plombage involved the extrapleural insertion of a “plombe” to collapse the lung
- Such plombes included
- Sanatorium movement began slower in US than Europe
- Once started, many opened and became a major way of treating TB
- In 1953, 839 TB sanatoria were operating in the USA stressing
- Diet
- Regimented exercise
- High altitude (where possible)
- Bedrest
- Sunlight
- Cold air
- Chemotherapy
- Streptomycin was the first, widely-used, effective anti-tuberculous agent (1946)
- Subsequently, isoniazid (1952), pyrazinamide (1954), cycloserine (1955), ethambutol (1962) and rifampin (1963) were introduced
- In the 1980s, drug-resistant strains emerged and the number of cases increased
- Multiple drug treatment regimen is the standard of care: usually isoniazid, rifampin, pyrazinamide, and either ethambutol or streptomycin
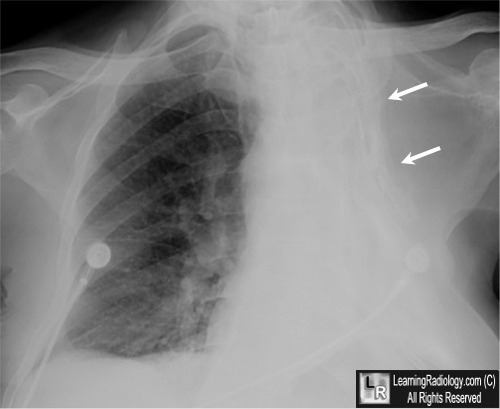
Thoracoplasty for TB. Frontal radiograph of the chest demonstrates a pathognomonic
appearance
of the left chest wall in which the upper 6-7 ribs have been intentionally displaced medially as part of"collapse therapy" used for TB before anti-tuberculous drugs (white arrows).
The hemithorax
is opaque from a combination of scarring and the surgery.
For this same photo without the arrows, click here
For more information, click on the link if you see this icon 
|
|
|